Volunteer Activity
Health and Social Care
From 2009, FOM was able to recruit health volunteers to assist in developing the health service structures in order to deliver the Maldivian government's mission: to “provide affordable, accessible and quality health care for all” as a human right. Some of the ways Mohamed Nasheed's government intended to do this were through establishing internationally accepted standards of health care; improving the quality of health services; establishing better referral systems and high quality regional health centres; assuring health care training opportunities to Maldivians; reducing the costs of health care; setting up an inclusive social health insurance system; and encouraging private sector participation in health. The government also made a great commitment to tackling substance misuse, which is a major social problem. Some of the ways it intended to do this were through eliminating the illegal supply of narcotics and other illicit drugs into the Maldives and establishing a comprehensive and coordinated national response to combat substance abuse. Particular goals were for health care to be more accessible to its disparate population, more sustainable in the face of a tough economic climate, and better able to deal with specific social problems such as substance misuse. FOM recruited 14 health professionals to carry out specific projects. Unfortunately, the over-throw of the elected government has made it increasingly difficult for the volunteers to function and most of the health volunteers, who worked closely with the Ministry of Health and Family, have all had to leave. Some of their reports are below:
Community Health Specialists
 Tom Heller, GP, and Gwen Wilson, Community Nurse / Health Visitor / Midwife were the first pilot health volunteers. They were based in the southern atoll of Huvadhoo for 2 weeks and during this time they worked flat-out to inspect the health facilities, check the medical records and talk to staff at all levels across 4 islands in the area. They also visited Male’ to gain a greater understanding of the country’s broader health needs. They discussed health and environmental issues with a wide range of people, including health professionals, Government officials, students and young people as well as many other ordinary citizens, and the President himself.
Tom Heller, GP, and Gwen Wilson, Community Nurse / Health Visitor / Midwife were the first pilot health volunteers. They were based in the southern atoll of Huvadhoo for 2 weeks and during this time they worked flat-out to inspect the health facilities, check the medical records and talk to staff at all levels across 4 islands in the area. They also visited Male’ to gain a greater understanding of the country’s broader health needs. They discussed health and environmental issues with a wide range of people, including health professionals, Government officials, students and young people as well as many other ordinary citizens, and the President himself.
They were able to explore possibilities for future volunteer health worker placements from the United Kingdom through the auspices of Friends of Maldives. In particular, they noted that further incremental improvements to the health of the people of the Maldives would come about through development of the education and training of Maldivian nurses, midwives, traditional birth attendants and community health workers, and through changes to the physical environment, including:
- Improved standards of refuse collection and waste disposal
- Sewerage treatment before discharge into the surrounding water
- Cleansing of domestic rainwater supply and storage mechanisms
- Targeting mosquitoes through breeding site reduction, selective killing of adult mosquitoes and community level health education and involvement in vector control activities
Tom Heller has continued to play an active part in recruiting and advising health volunteers to the Maldives.
Tom’s two full reports can be viewed at :
 Gwen Wilson is continuing her work by assisting in the development of a Community Public Health / Health Educator role. The proposal can be viewed at : Development of a community public health
Gwen Wilson is continuing her work by assisting in the development of a Community Public Health / Health Educator role. The proposal can be viewed at : Development of a community public health
Public Health
May 2010
Andrew Lee, Clinical Lecturer in Public Health / GP travelled to the Maldives as part of the Sheffield Collaborative. He was primarily based at Hulhumale hospital and spent the first part of his placement examining local public health activity and opportunities. He visited the Centre for Health and Disease Control, which is akin to a UK Public Health Department, and looked at scope for its greater integration with the main hospital staff. With his prior experience in running primary health care and tuberculosis control programmes overseas, and expertise in tropical medicine, he was ideally placed to advise on practical ways in which the hospital could play a greater role in health promotion and education, and disease prevention. As an example, he undertook smoking cessation and drug awareness training with the local police, and suggested ways the hospital could engage more effectively with the local healthy population, through workshops in schools etc.
Andrew’s Report on Public Health Services, and observations from Hulhumale Hospital can be viewed at Public Health Report 2010
 Andrew spent the second half of his placement running a quality improvement training programme (see below). He was also able to take a little time out from his hectic schedule to enjoy a sea fishing trip, with his colleague, Paul Harvey.
Andrew spent the second half of his placement running a quality improvement training programme (see below). He was also able to take a little time out from his hectic schedule to enjoy a sea fishing trip, with his colleague, Paul Harvey.
Child Health
David Campbell, Consultant Paediatrician went to the Maldives as part of the Sheffield Collaborative. Besides a short stint in Addu, he was mainly based at Gn Hospital, Fuvamulah. His work was split between clinics where he saw many children with diverse health needs, and teaching of hospital staff. He carried out a programme of teaching in neonatal resuscitation, appropriate use of drugs (antibiotics) and exclusive breast feeding, which had been identified as priority areas by Mohammed Saeed, the Area Medical Officer in charge for the Southern Atolls. Laminated flow sheets are now on the delivery ward and the side ward in theatres including a crib sheet for drug doses for term babies. David also did a medical update on gastroenterology, his primary speciality, as a separate teaching session.
 David did much of the training with his wife, Fiona Campbell, who is a Research Associate at Sheffield University, aswell as a qualified Health Visitor and District Nurse.
David did much of the training with his wife, Fiona Campbell, who is a Research Associate at Sheffield University, aswell as a qualified Health Visitor and District Nurse.
David’s reports on Paediatric Services and Child Protection can be viewed at Paediatric report 2010
Whilst David was in the Maldives, he was asked by Mariyam Ali, Deputy Health Minister, to look at local child protection practices. Since David provides part of the child protection service in Sheffield, in conjunction with a police medical officer and specialists in child protection, he was able to make useful recommendations regarding scope for improving services for vulnerable children. He noted that whilst Social Services had robust written procedures for dealing with suspected child abuse, there were gaps in its delivery. For example, there was often no paediatrician or gynaecologist available to examine a child. Also, the process between reporting and prosecuting did not appear to be working well in child protection cases in Fuvamulah. Police did not always collect statements from doctors and witnesses, photographic evidence was not routinely used and forensic specimens were often unuseable, leading to weaknesses in documentation of injuries. Further investigation is recommended to focus on medical report writing, police liaison and law enforcement work to bolster their approach to these problems.
The Child Protection Report can be viewed at Child Protection in Fuvahmulah 2010
Specialist Services
October 2009
 Somma Ahir Cardiac Nurse Specialist worked at the Indira Gandhi Memorial Hospital in Male' for 1 month. She undertook patient care and staff development in the Intensive Critical Care Unit and also did a large amount of training throughout the hospital. She developed resource files and clinical guidelines to improve the quality of care for critically ill patients. Somma’s report of her experiences can be viewed at Cardiac Nurse Report
Somma Ahir Cardiac Nurse Specialist worked at the Indira Gandhi Memorial Hospital in Male' for 1 month. She undertook patient care and staff development in the Intensive Critical Care Unit and also did a large amount of training throughout the hospital. She developed resource files and clinical guidelines to improve the quality of care for critically ill patients. Somma’s report of her experiences can be viewed at Cardiac Nurse Report
April 2010
Graham Merrick Consultant Maxillofacial Surgeon worked at the Indira Gandhi Memorial Hospital for a short placement, as a self funded volunteer, whilst he was in the Maldives as navigator for the Zero Degree crossing. He undertook outpatient clinics, where he saw many patients from various islands; he performed operations on all the patients identified from the clinics as requiring surgery within his sphere of expertise; and he increased the confidence and scope of practice of the dentists at IGMH through guided teaching and supervised surgery.
April – May 2010
James Forsey, Consultant Obstetrician, worked in both Hulhumale and Addu. He met with many stakeholders in the provision of maternity services and assessed scope for positive change. He did a large amount of multidisciplinary teaching, helped develop written protocols and regular team meetings as a fora for reviewing notable cases. His recommendations can be viewed at Obstetric Report 2010
Substance Misuse
December – February 2009/10
Jonathon Drewhurst and Jennifer Drife, Drug Rehabilitation Psychiatrists, were placed around Male’ for 3 months. During that time they liaised with, and held workshops with the Ministry of Health, the police, relevant NGOs and hospital staff. Some of the projects they worked on included investigating suicides and mental health problems amongst drug users, examining data relating to methadone clinics, surveying attitudes to needle sharing in injecting users and conducting a training programme for local drug rehabilitation counsellors.
They presented their findings to both the Vice President of the Maldives, who is taking an active lead in problematic drug-use issues, and the Drugs Council.
May 2010
 Paul Harvey, GP with expertise in community based substance misuse management went to the Maldives as part of the Sheffield Collaborative.
Paul Harvey, GP with expertise in community based substance misuse management went to the Maldives as part of the Sheffield Collaborative.
Paul was based with the Drugs Prevention and Rehabilitation Service and visited a wide range of facilities and stakeholders involved with drug rehabilitation. He visited the detox unit in Villigilli, the residential rehabilitation facility at Himmafushi and the HIV control project.
He was also able to discuss the dreams of 2 key NGOs, Society for Women Against Drugs (SWAD) and Journey, who strive for a cognitive approach to rehab, rather than a therapeutic community, and for better collaborative working between the NGO’s, and also between NGO’s and statutory providers. Paul was impressed by the range of sports, arts and craft activities available, alongside counselling and family therapy.
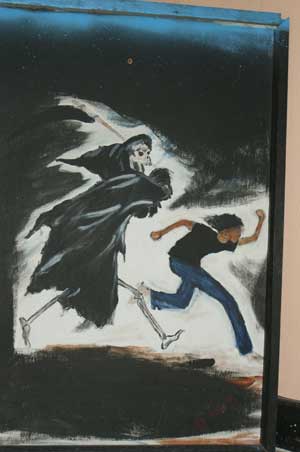
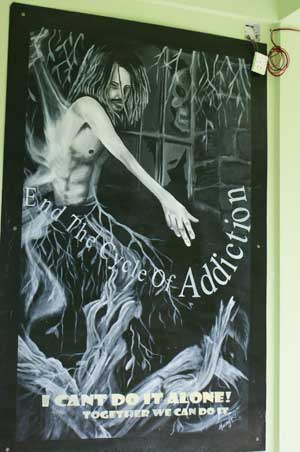

During meetings with Mariya Ali, Deputy Health Minister, Paul was able to discuss links between substance misuse, mental health and child protection, and potential for establishing a national drugs telephone hotline, which could refer clients to community teams if appropriate.
To examine drug links with mental health and broader society, Paul met with psychiatrists and Family Protection staff at IGMH, aswell as 40 Hulhumale police officers and members of the Crime Prevention Group.
Paul also met with Mohamed Waheed, Vice President of the Maldives, who had previously expressed an interest, to Friends of Maldives, in meeting volunteers dealing with substance misuse issues, as one of the government’s 5 key pledges. He was very enthusiastic about piloting a community team to address drug care, and keen to listen to Paul’s suggestions:
- Joint drug protocols for all treatments to allow effective management by more professionals
- Community detox.
- Establishment of community drug care teams for each atoll, perhaps being part of larger community mental health or social work teams
- Rehabilitation of recovering drug misusers into employment and society
- Drug teams for prisons, including ways to address mental health issues
- Halfway house facilities for recovering addicts
- Examine the law which stops drug treatment in pending court cases
- Look at code of conduct for all drugs workers with agreed training and confidentiality.
- Consider needle exchange schemes as a means to reduce infection and improve safety.
Paul’s reports on can be viewed at Substance Misuse 2010 and Current Model of Drug Care 2010.
Whilst Paul was collaborating with Andrew Lee, they were able to further explore ways to raise the profile of public health as a specialty in the atolls, to change the population’s expectations regarding accessing care, and providing a good enough primary care service that patients do not self-refer to specialists.
Quality Improvement
May 2010
Andrew Lee, Clinical Lecturer in Public Health / GP and Fiona Campbell, Research Associate / Health Visitor / District Nurse also went to the Maldives as part of the Sheffield Collaborative. They ran extensive training programmes in Quality Improvement Through Audit and Research. They both assisted delegates to apply the principles of audit and research to practical situations, which the delegates wished to explore further.
Andrew Lee delivered a national training programme to multidisciplinary health staff in conjunction with Quality Improvement Division (QID) staff.
Sessions were delivered as lectures and interactive workshops, including:
- Introduction to quality improvement and patient safety
- Clinical audit
- Developing criteria and standards/Evidence-based practice
- Data collection and analysis
- Implementing change
- Mapping the care pathway/Problem tree analysis
The participants described their audit topics and plans for the coming year, and were issued with certificates by Dr Yasir, Director General of Health Services. Andrew will be supporting the participants, via the internet, in executing their projects. It is hoped that they will report back to QID on their completed audits in the next 12 months, so they can be compiled, published, and disseminated throughout the country.
Andrew also spent time with QID looking over the regulatory inspection checklists and discussed the process for developing standards and protocols. The Quality Improvement Report can be viewed at Quality Improvement Report 2010.
 Fiona Campbell was mainly based in Fuvahmulah, where she carried out extensive training with the local nurses and other staff at Gn Hospital. She creatively used home made videos and pictures to stimulate ideas for audit, and supported nurses in data collection relating to their chosen areas of enquiry. Fiona enhanced the training with quizzes and prizes, participated in Nurses Day, with a costume made for her by the local nurses, and was a source of mentorship for the nurses whilst she was on the island.
Fiona Campbell was mainly based in Fuvahmulah, where she carried out extensive training with the local nurses and other staff at Gn Hospital. She creatively used home made videos and pictures to stimulate ideas for audit, and supported nurses in data collection relating to their chosen areas of enquiry. Fiona enhanced the training with quizzes and prizes, participated in Nurses Day, with a costume made for her by the local nurses, and was a source of mentorship for the nurses whilst she was on the island.
The nurses were very engaging as they had few educational opportunities and lots of ideas which they wished to develop. One area they were interested in was breast feeding, so Fiona took to a motorbike to interview local people in the community, with the nurses, in order to carry out a breast feeding project. This work culminated in a report on breast feeding and growth of children: Fiona’s report of the work she did with the nurses is available at Breast feeding and growth survey 2010.
Fiona also delivered some teaching with her husband, David Campbell, Consultant Paediatrician, aswell as assisting Andrew Lee in delivering some of the training for the course arranged by QID.


